A 70 yr old male patient with heart failure.
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
Date of admission:-27/11/2021
CHIEF COMPLAINT:-
A 70 yr old male patient farmer came to the opd with c/o : Sob since 10 days.
Scrotal swelling since 12 days
Generalised swelling of body since 12 days
Facial puffiness since 12 days
C/o constipation since 12 days (passing stools only on medication).
NORMAL ROUTINE OF PATIENT:-
Patient use to wake up at 5AM in the morning daily. He used to brush and have a cup of tea.
He consumes breakfast around 8-9 am .
He goes to farming at 10 am and work until 4pm .He takes his lunch around 1-2 pm .
Then he returns home watches TV and have dinner by 7 pm and goes to sleep by 8 pm.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 1 month back.
Then he developed swelling of right leg upto the knee and facial puffiness.
15/10/2021
He visited a doctor in miryalagudem and was treated for the same and symptoms were subsided.
16/10/2021
On USG - there was mild left pleural effusion seen .
He was diagnosed for chronic kidney problem on testing.
On 15/11/2021
Patient developed gross scrotal edema, anasarca and decreased urine output.
ON 16/11/21-
He visited the doctor and
on usg -scrotal wall cellulitis
RBS- 279
Blood urea- 97
Raised serum creatinine-3.6mg/dl
Serum Uric acid- 7.6mg/dl
LFT- within normal range, albumin-3.5
He was treated with-
Inj.cefaoish (cefoperazone and sulbactam)
T.metrogyl
T.dytor 10mg
T.amlong 10mg
T.Nodosis
T.nephrosave
Nebulisation with formonide
T.ecospirin 75mg
Inj.hai 12u———10u
T.chymeral forte
Scrotal support bandage
And 1 PRBC TRANSFUSION DONE.
On 17/11/21-
Hb- 9.4
Blood urea- 96
Serum creat- 2.6
On 28/11/21
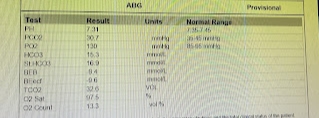
Pt has severe pulmonary edema.Hypoxia with hypercapnia(Refractory acidosis).
Patient developed cardiac arrest around 10 pm and recovered after cpr.
He was kept on ventilation since then.
PAST HISTORY:
H/o RT LL CELLULITIS (due to DM-II) 14 months back. (Patient use to scratch his leg frequently.)
Got treated with various antibiotics (meropenem etc) and tramadol for pain for around 3-4 months. Later got skin grafting done.
He is k/c/o type -II diabetes since 20 yrs .He is on medication since then.From past 8 yrs he was on insulin therapy.
PERSONAL HISTORY:
Mixed diet.
Appetite-normal
Addictions- none
Bowel and bladder movements-
He was normal until 16/11/21 when he developed gastritis and constipation and wouldn’t pass stools for 4 days. And on taking medication he would pass stools.
Till now (from 16/11-27/11) stools passed- 5 times.
Micturition - decreased urine output since 5 days.
FAMILY HISTORY:
No significant Family history .
GENERAL EXAMINATION:
Pallor-present
Icterus-absent
Edema- generalised body edema (pitting type) present
NO clubbing,cyanosis, lymphadenopathy
Vitals:
pulse-102beats/min
Rr-19cpm
BP- 110/80 mmHg
spo2 - 95%
SYSTEMIC EXAMINATION:-
CVS
s1,s2 heard
RS :
BAE + ,NVBS
P/A-
soft, non-tender
No guarding or rigidity, BS +
B/l scrotal edema (Scrotum enlarged diffusely) ; PENILE EDEMA +
No local rise of temperature
No tenderness, no c/o cellulitis
CNS:
NAD
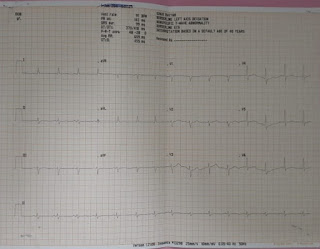
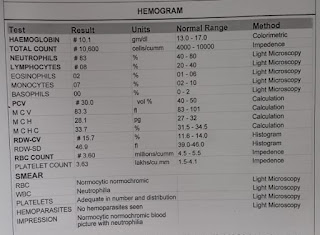
INVESTIGATIONS:
PROVISIONAL DIAGNOSIS :-
HFEPEF WITH moderate MR+/AR+/TR+ with k/c/o DM with scrotal edema , CKD.
Left Ventricular Failure (may be due to coronary artery disease).
TREATMENT:-
T.LASIX 40mg BD
Inj. MONOCEF 1gm/IV/BD
T. OROFER-XT PO OD
T.NODOSIS 500mg BD
T. SHELCAL-CT PO OD
NEB WITH DUOLIN 8th hrly, BUDECORT 12th hrly
T.ECOSPRIN-AV 75/10mg
T.HYDRALAZINE 12.5mg BD
STRICT I/O charting
FLUID AND SALT RESTRICTION
INJ.HAI S/C ACC TO GRBS
SCROTAL SUPPORT
BP/PR/TEMP CHARTING 4th hrly
After admission into ward the patient developed SOB AND BECAME TACHYPNOEIC(28cpm) with a BP OF 150/100. B/L IAA crepts and wheeze present.
Pt was given lasix 40mg and nebulisation with budecort and Duolin.
Pt then Shifted to AMC and continued with nebulisation.
Patient expired on 29/11/2021 Monday at 9:40pm.

















Comments
Post a Comment